How to treat congestive cardiac failure – sudden heart failure. You have often heard people say
that such-and-such a person died of heart failure. As soon as we hear the name “heart failure,”
we think of someone’s death. Although, a medical perspective on heart failure differs from what
people believe it to mean,
Definition of congestive cardiac failure
In medical science, heart failure occurs when the heart cannot pump enough blood
(which our body needs) regularly. Can you say ”
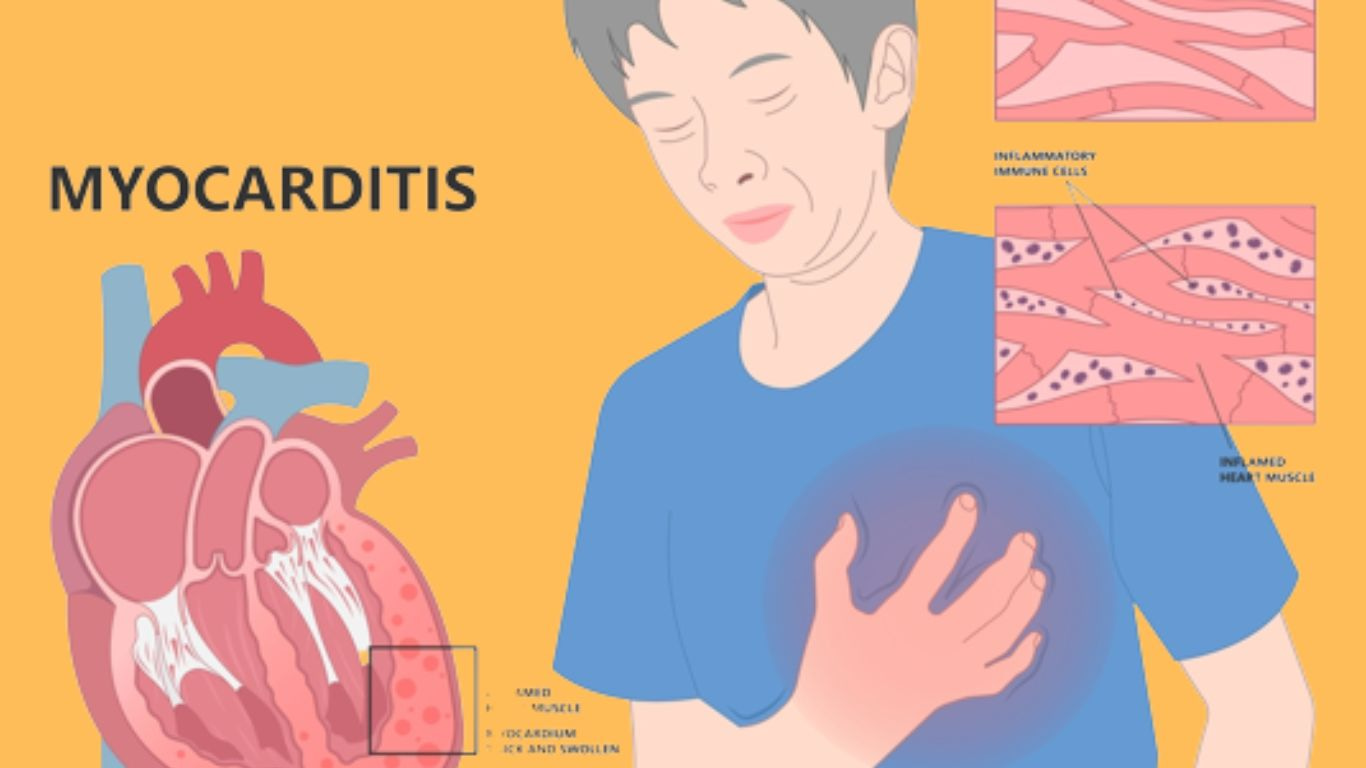
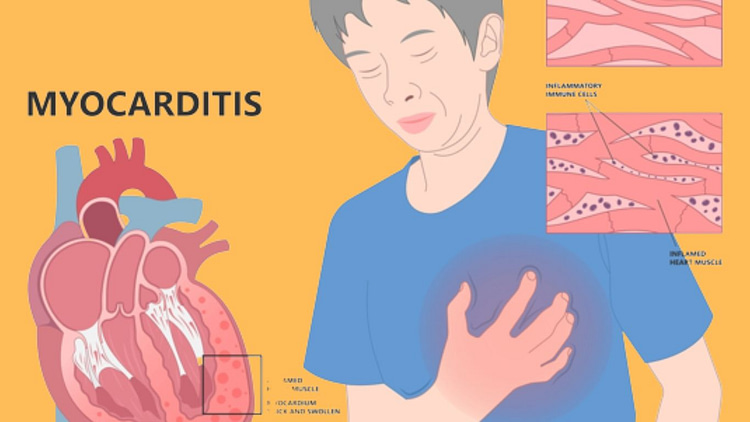
Congestive heart failure causes
- Due to infarction.
- Due to inflammation of the heart.
- Due to ischemic diseases. These are diseases in which the heart has adequate (Blood cannot be found.)
- Due to blood pressure.
- Due to respiratory diseases.
- Due to a heart valve defect.
- Due to defects in the nodes of the heart. (The nodes that generate a kind of electricity for the heart are – )
Obviously, if the generators are damaged, the pumping performance of the heart will be
affected and it will become weak, so we will say that the heart has failed.
Cardiac failure symptoms
The brain and kidneys are deficient in blood.
The body begins to lose water. Swelling in the face, feet, legs, and abdomen.
Cardiac failure treatment
Homeopathy should be treated based on the symptoms. By the way, there are many heart medicines.
-
Aurum Metallicum 30
Aurum metallicum Aurum 30 is a useful homeopathic treatment for cardiac problems.
-
Laurocerasus 30
Laurocerasus is one of the most effective homeopathic treatments for heart failure.
-
Crataegus Oxy
Crataegus is regarded as a heart tonic and beneficial in cases of heart weakness coupled with
oppression, sleeplessness, and sutures.
-
Cardus Marianus Q
Carduus marianus is an effective homeopathic remedy for heart failure.
-
Naja tripudians 30
Naja tripudians 30 can help with heart failure.
Congestive heart failure after triple bypass
It is possible to restore blood flow to a part of the heart by undergoing bypass surgery,
also known as coronary artery bypass grafting. However, it does not stop the progression
of atherosclerosis (coronary heart disease), which causes fatty material to accumulate
in artery walls and restricts blood flow over time. After surgery, patients and medical
professionals should work together to address the underlying atherosclerosis and other
risk factors that can lead to heart disease progression. (For tips on reducing cardiac
risk factors, see below.) This theme overview focuses on recommended treatments
after CABG that can be helpful.
Lower the risk of experiencing complications related to coronary heart disease,
such as a second heart attack or death. Help someone feel more energetic and
improve their overall well-being. Also, there is a detailed explanation of coronary
artery bypass graft surgery provided separately.
Congestive heart failure after Covid-19
It is possible that COVID-19 survivors may experience changes in the structure of their
hearts as well as a higher risk of cardiovascular disease. An investigation was conducted
to determine whether there is a possibility of developing heart failure after recovering
from COVID-19. Data were collected by searching MEDLINE and Scopus for all
publications reporting the risk of incident heart failure in recovered COVID-19 patients
up to September 1, 2022. The risk of incident heart failure following COVID-19 was
analyzed using a random-effects model with a 95% confidence interval. Statistical
heterogeneity was measured by the Higgins I2 statistic. There were 21,463,173
patients (58.7% male) who were examined, as well as 1,628,424 who were diagnosed
with COVID-19 and 19,834,749 who were controls. E study followed up with patients
for an average of 9.2 months and found that 1.1% of them developed CI post-COVID-19.
This was determined through a random-effects model with a confidence interval of
95% (0.7-1.6) and an I2 of 99.8%. During the same period, patients who had recovered
from COVID-19 had a higher risk of developing incident HF, with a hazard ratio of 1.90
and a confidence interval of 95% (1.54-3.24), p<0.0001, and an I2 of 96.5%.
Meta-regression showed a direct correlation between incident HF risk and
age (p=0.001) and hypertension (HT) (p=0.02). However, when the length of
follow-up was used as a moderator, an inverse correlation was observed (p=0.01).
It has been found that long-term COVID-19 infection increases the chance of
developing heart failure by 90%. Early post-acute phase and HT history were
directly associated with this risk.